Objective
Peripheral blood stem cells serve as the primary source of hematopoietic stem cells for both autologous and allogeneic stem cell transplantation. Granulocyte colony-stimulating factor (G-CSF) stands as the most commonly employed mobilizing agent in clinical practice. While the majority of donors receiving G-CSF mobilization demonstrate high mobilization efficiency, there remains a subset of donors who fail to yield a sufficient quantity of hematopoietic stem cells. Inefficient mobilization not only leads to wastage of valuable resources but also significantly impacts transplant outcomes for recipients. Therefore, addressing the challenges associated with predicting mobilization outcomes, optimizing donor selection strategies, and further enhancing mobilization approaches is of paramount importance.
Methods
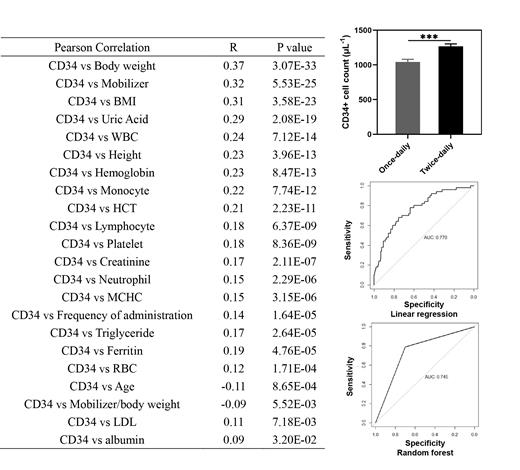
In this study, we conducted a retrospective analysis of mobilization data from 1008 donors who underwent hematopoietic stem cell mobilization using G-CSF at the Bone Marrow Transplantation Center, the First Affiliated Hospital, Zhejiang University School of Medicine, over the past 5 years. We meticulously examined the correlation between mobilization outcomes (quantified by the quantity of collected CD34+ cells) and various factors, including mobilizing agent usage, demographic data, complete blood count, and blood biochemistry.
Furthermore, we harnessed the power of machine learning algorithms, such as linear regression, decision tree, and AdaBoost, to develop a robust scoring model capable of predicting mobilization outcomes. The primary objective of this model is to furnish a predictive tool for assessing mobilization outcomes with accuracy and precision.
Results
(1) Prior to receiving G-CSF, several factors exhibited a significant positive correlation with the quantity of CD34+ cells in the collection: donor's body weight (R=0.37, p<0.001), peripheral blood leukocytes (R=0.24, p<0.001), hemoglobin (R=0.23, p<0.001), monocytes (R=0.22, p<0.001), lymphocytes (R=0.18, p<0.001), platelets (R=0.18, p<0.001), red blood cells (R=0.12, p<0.001), neutrophils (R=0.15, p<0.001), hematocrit (R=0.21, p<0.001), mean corpuscular-hemoglobin concentration (R=0.15, p<0.001), low-density lipoprotein (R=0.11, p<0.01), albumin (R=0.09, p<0.05), ferritin (R=0.19, p<0.001), triglycerides (R=0.17, p<0.001), creatinine (R=0.17, p<0.001), and uric acid (R=0.29, p<0.001).
(2) Age exhibited a significant negative correlation with the quantity of collected CD34+ cells in the collection (R=-0.11, p<0.001).
(3) When the total dose of G-CSF administration was fixed, mobilization with twice-daily dosing yielded superior results compared to once-daily dosing (collected CD34+ cell count: 1268/μl vs. 1044/μl, p<0.001).
(4) The ratio of G-CSF dosage to body weight demonstrated a significant negative correlation with the quantity of CD34+ cells (R=-0.09, p<0.01). Mobilization with a ratio of 6-7 μg/kg/day showed better results compared to a ratio of 7-12 μg/kg/day (p=0.07).
(5) A scoring model was developed using machine learning methods to predict the mobilization outcomes of donors. Validation on the test dataset exhibited a high predictive ability of the model (AUC>0.7).
Conclusion
This study provides valuable insights for selecting hematopoietic stem cell donors and serves as a reference for future strategies aimed at improving mobilization outcomes. The identified factors, such as donor weight, peripheral blood parameters, G-CSF dosing regimen, and the ratio of dosage to body weight, can be considered when selecting donors and optimizing mobilization protocols. By incorporating machine learning techniques, a scoring model was developed, demonstrating a high predictive ability that can assist in forecasting mobilization outcomes for potential donors. These findings contribute to the optimization of donor selection and mobilization strategies.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal